Cure for chronic/recurring infections?
 Ever wonder why you can’t seem to get rid of your sinus infection? Or it goes away for a little while and then comes back again? Maybe for you it’s not sinus infections but urinary tract infections? You take antibiotics for weeks on end and as soon as you stop them the infection comes back?
Ever wonder why you can’t seem to get rid of your sinus infection? Or it goes away for a little while and then comes back again? Maybe for you it’s not sinus infections but urinary tract infections? You take antibiotics for weeks on end and as soon as you stop them the infection comes back?
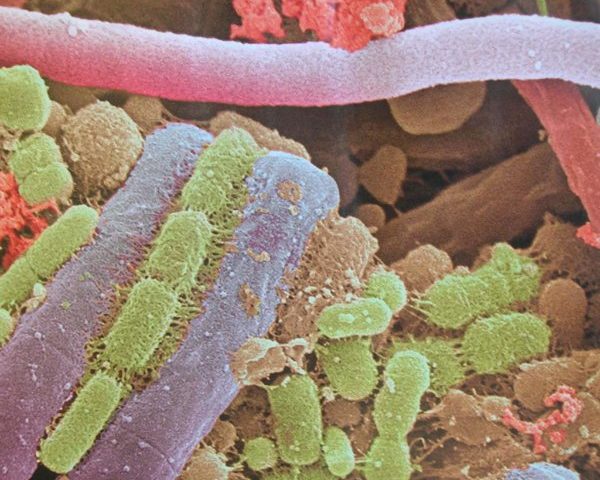
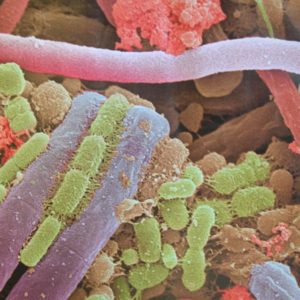
Chances are good that pathogens creating your infection have coated themselves in a biofilm, making them extremely hard to treat. What’s a biofilm? It’s a slimy, glue-like membrane composed of polysaccharides made by bacterial and fungi. Within that film one or more types of bacteria and/or fungi share nutrients and DNA and undergo changes to evade the immune system. Since it requires less oxygen and fewer nutrients and alters the pH at the core, the biofilm is a hostile community for most antibiotics. In addition, the biofilm forms a physical barrier that keeps most immune cells from detecting the pathogenic bacteria. (1)
According to the National Institutes of Health, more than 80% of human bacterial infections are associated with bacterial biofilm. This problem has long been known to hospitals dealing with medical implants, vascular grafts, and severe dermal wounds. Biofilms often are involved in ear infections, sinus infections, chronic tonsillitis, dental plaque, endocarditis, lung infections in cystic fibrosis, kidney stones, biliary tract infections, urinary tract infections, bone infections, and chronic wounds. Biofilms also have been linked to both Crohn’s disease and ulcerative colitis, and are thought to impede treatments involving infections, such as E. coli and H. pylori, in the digestive tract.
Unfortunately, biofilms often are difficult to diagnose. They don’t show up in swabs or stool samples, and they are not easily cultured.
If you suspect a biofilm may be involved in a tough-to-treat infection, what can you do? Find a biofilm disruptor. It can be taken with antibiotics or antimicrobial herbal treatments.
Interestingly, some of them are commonly found in health food stores.
Nattokinase, an enzyme produced from fermented soybeans, breaks down fibrin and fibrin is part of the matrix of some biofilms. It has been used extensively as a coating on implants to help prevent biofilms from forming.
N-acetylcysteine (NAC) occurs naturally in the body, being derived from the amino acid l-cysteine. It both increases glutathione (the body’s most potent antioxidant) and breaks down mucus. It’s effective against biofilms on prosthetic devices. (1)
Colloidal silver is effective in treating topical biofilms, though there is little to no research showing its effectiveness as a biofilm disruptor internally.
There also are combination products designed to break down biofilms. Chris Kresser, founder of Kresser Institute and a widely known natural health practitioner/teacher, recommends Klaire Labs InterFase Plus or Kirkman Biofilm Defense. Both are either available or can be ordered at Ruth’s.
Kresser also recommends using antimicrobial treatments following, and along with, biofilm disruptors. That may be an antibiotic prescribed by your doctor or mixtures of potent herbs. For example: berberine, artemisinin, black walnut hulls, oregano oil, goldenseal, echinacea. Designs for Health G.I. Microb-X or Biocidin by Bio-Botanical Research are two such products that can be ordered at Ruth’s.
Be aware that when using antimicrobial treatments, patients may get a die-off reaction. When bacteria die, they release toxins that can leave you feeling tired, achy, sleepy. Using activated charcoal can help absorb the toxins and lessen the reaction.
REFERENCES:
1. BioFilms