Diet & supplements can help recovery
By Sue Cummings
I recently listened to a podcast interview of a doctor I really admire, Dr. Robert Rountree, a long-time functional medicine doc and the recipient of the Linus Pauling Functional Medicine Award in 2015. I’ve attended workshops with Dr. Rountree in the past, and I know him to be one smart cookie. So I was excited to hear him sharing his work on non-alcoholic fatty liver disease (NAFLD), a condition that is affecting an alarming number of Americans.
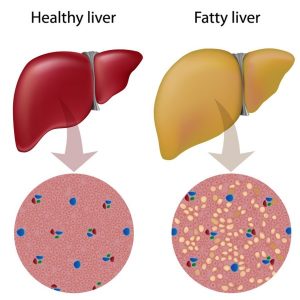
Current studies indicate that about one-third of the U.S. population has some degree of NAFLD, where more than 5% of liver tissue is fat. Roughly 10% of healthy appearing children have NAFLD, with 80% of obese children affected. Forty to 90% of obese adults have NAFLD and up to 70% of type 2 diabetics have it. In studies, those with fatty liver disease have a 70% higher mortality rate compared with controls, usually caused by a cardiovascular event.
Left untreated NAFLD generally leads to chronic liver inflammation and 5 to 8% of those with chronic liver inflammation develop liver cirrhosis within five years. It’s the third most common indication for liver transplant.
Sadly, most people won’t know they have NAFLD until routine blood work indicates a high ALT liver enzyme.
Risk Factors/Indicators
So who’s at risk for getting non-alcoholic fatty liver disease? Apparently a lot of Americans. There’s a high association with insulin resistance and obesity, but it can also appear in those who are thin. Indicators are:
- Type 2 diabetics
- The obese
- It can occur in lean people, especially if there is sarcopenia (muscle loss with aging)
- Diet high in refined carbohydrates, especially high fructose corn syrup
- High homocysteine levels
- Hypothyroid
- Sleep apnea
- Polycystic Ovarian Syndrome
- Gastric Bypass
- Chronic corticosteroid use
- Methotrexate use
- Chronic inflammatory conditions
- Sedentary people
- Choline and/or folate deficiency
Treatment
Rountree noted that when you track consumption of high fructose corn syrup with fatty liver, they go up in parallel. It goes up in parallel with obesity as well. Fructose, he explained, doesn’t raise blood sugar but it does cause insulin resistance, and that turns on genes in the liver that create new fat as well as inflammation.
That’s why Rountree’s number one recommendation for those with NAFLD is to stop eating processed foods, especially high fructose corn syrup. In addition, he recommends losing weight, at least 5% of body weight to lose fat in the liver, along with exercising at least 150 minutes a week.
He’s also big on supplements shown to improve fatty liver. Rountree explains that you need choline to make phosphatidylcholine (PC) in the liver. The PC is then used in the very low density lipoprotein (VLDL) to pack its lipids and ship them out of the liver. If you don’t have enough phosphatidylcholine, then those fats can’t be shipped out and they accumulate. And Rountree maintains that many Americans are deficient in choline. In addition, he uses: curcumin (500 mg twice daily), Sunfiber (5-8 g. daily), berberine (500 mg twice to three times daily) and vitamin E (800-1,000 IU daily). With those he says he’s getting good results. (He also likes Meriva, which contains both curcumin and phosphatidyl choline.)
Given that there is NO approved pharmaceutical therapy for NAFLD, Rountree’s clinical pearls are welcome news.
REFERENCE: