Tips from experts to better protect your heart from lethal disease

Heart disease is the No. 1 killer of both men and women in the United States. If you look at the Centers for Disease Control map on heart disease, the South has some of the highest death rates from cardiovascular causes, though Madison County appears a bit better than surrounding areas.
Nonetheless, there’s clearly room for improvement.
What are the risk factors? Smoking, high blood pressure, diabetes, high cholesterol (though many docs in the functional medicine community would say it’s not so much high cholesterol but oxidized cholesterol, indicating inflammation is as big a factor as just cholesterol), a big waistline, being sedentary, eating the Standard American Diet, age (55 or older for women), and having a family history.
Some of the solutions to lower risk factors are obvious: don’t smoke, lose weight, limit your sugars, and exercise regularly. But there’s a lot more you can do to improve your heart health.
Dr. Mark Houston
Dr. Mark Houston, one of the top physicians treating hypertension in the US and practicing at St. Thomas Hospital in Nashville, focuses on improving chronic inflammation, oxidized cholesterol, high blood pressure, high blood sugar, and high insulin.
Most heart disease starts with inflammation, from any cause, that becomes chronic. That gives it the opportunity to damage blood vessels and increase inflammation even more. Houston says one of the most prominent indicators of inflammation is high-sensitivity C-reactive protein (HS CRP), which can be measured by a blood test.
What increases your risk for chronic inflammation? According to Houston, increased intake of refined carbohydrates, increased intake of trans-fatty acids, smoking, lack of sleep, lack of exercise, chronic infections, heavy metals, and chronic autoimmune and inflammatory diseases.
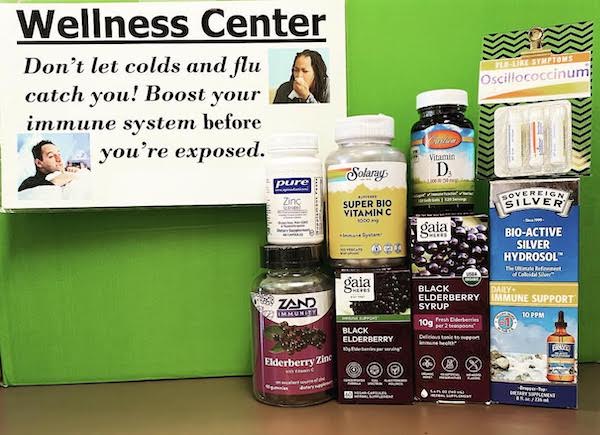
What can you do to improve your inflammation score? Obviously, improve the above situations where you can. He also recommends choosing from several anti-inflammatory/antioxidant supplements: Omega-3 oils, curcumin, CoQ10, vitamins C/D/E, N-acetyl cysteine, selenium, zinc, and more.
According to Houston, at lot of cholesterol testing is out of date. He says if you are not getting a test that measures the size of your cholesterol particles, not just the numbers, along with including the newer CVD marker ApoB, it’s inadequate. Particle size matters because big, fluffy particles are usually less damaging to arterial walls than smaller, denser particles. ApoB (apolipoprotein B) is a structural protein that constitutes a major component of VLDL. It is now thought to be a good marker of the number of damaging particles you have in circulation.
What to do if you get an advanced cholesterol test and you find too many small particles, your ApoB is high, or your triglycerides are too high? Houston recommends: cutting back on refined carbohydrates, eliminating all trans-fats (found in processed and deep-fried foods), taking omega-3 oils from fish or algae, drinking green tea or taking an EGCG supplement, along with taking resveratrol to reduce oxidation.
While all the doctors recommend exercise, Houston looks at exercise not as a way to burn calories, but as a way to talk to your genes and turn on healthy hormones. “Higher intensity exercise gets the muscles talking most. Exercise using full body movements, incorporating great amounts of muscles, requiring a combination of strength and endurance, and forcing the muscles to shout out a unique message that sets in motion a powerful muscle-building, fat burning, anti-inflammatory, and brain-stimulating effect.” He recommends exercising in the morning on an empty stomach, doing weight-training followed by aerobic training intervals.
Dr. Andrew Weil
Dr. Andrew Weil breaks down cardiovascular disease into more specific categories and then lays out suggestions for each. For atherosclerosis (plaque build-up in the arteries) Weil suggests the obvious solutions mentioned above and also eating a low-glycemic index diet, taking fish oil, and coenzyme Q10. He notes fish oils have been shown to lower triglycerides and inflammation while increasing HDL (the “good” cholesterol). CoQ10 is an antioxidant that Weil says helps protect LDL cholesterol from oxidizing and helps maintain healthy blood vessels.
Weil also mentions that high homocysteine levels in the blood (your doctor can test for this) is thought to contribute to plaque formation by damaging the arterial wall. Weil suggests eating more foods that contain B vitamins (green veggies, beans) and supplementing with a B-complex high in folic acid to bring homocysteine numbers down.
Dr. Mark Hyman
Functional Medicine Doctor Mark Hyman suggests the first step to reduce risk factors is to eat a healthy diet. He recommends avoiding white flour and sugar, increasing vegetable intake, and avoiding hydrogenated oils. He also recommends regular exercise and supplementing with a good multivitamin, fish oil, red yeast rice, plant sterols, and fiber.
Dr. Stephen Sinatra
Cardiologist Stephen Sinatra recommends taking at least 2 grams of high-quality fish oil daily to help prevent heart disease. He also recommends his “Awesome Foursome” of heart healthy supplements: CoQ10, magnesium, l-carnitine, and D-ribose. He suggests 50-100 mg of CoQ10 daily, but if you take a statin drug, he recommends 200-300 mg daily to better protect your heart (statin drugs deplete CoQ10).
L-carnitine helps move fatty acids (cell fuel) into the mitochondria (the engine in every cell). Sinatra suggests 1,000-1,500 mg in divided doses daily. Magnesium is needed in all reactions that help produce ATP (adenosine triphosphate), a molecule needed to supply energy to every cell. Sinatra suggests 400 mg daily with meals.
The last of Sinatra’s Foursome is D-ribose, a simple sugar that helps fuel regeneration of energy when your body can’t create it quickly enough, such as during heavy exercise or in people with ischemia. He recommends 5 grams daily prior to exercise.
Matthew Walker, PhD
A final note: While doctors here mentioned getting good sleep, there’s good reason to emphasize it more. Sleep researcher Matthew Walker, PhD, notes studies showing that adults 45 or older who sleep fewer than six hours a night are 200 percent more likely to have a heart attack or stroke during their lifetime, compared with those who sleep seven to eight hours a night. Poor sleep accelerates heart rate and increases blood pressure, encourages calcification of coronary arteries, and lowers growth hormone (which is needed to repair arteries). It’s a cascade of events that drive heart disease. Walker recommends setting aside a hard and fast 8-hour sleep opportunity every night.
REFERENCES
“Reverse Heart Disease Now” by Stephen T. Sinatra, MD
“What your Doctor May Not Tell You About Heart Disease” by Mark C. Houston, MD, MS
“Why We Sleep” by Matthew Walker, PhD